It is not the most pleasant substance. Its notorious smell and inextricable connection to potty humor make it an unappealing subject for many. However, its healing abilities offer a promising treatment for Autism Spectrum Disorder symptoms. What is this mysterious substance? Human fecal matter - also known as poop.
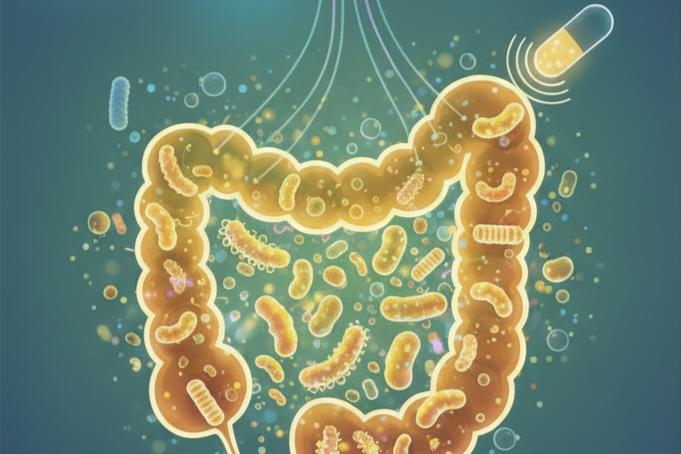
In a procedure known as fecal microbiota transplantation (FMT), human stool from healthy donors is introduced into a patient’s gut through a colonoscopy or a pill (Gupta et al., 2016). The healthy bacteria from the donor’s stool can positively impact the patient’s imbalanced intestinal microbiome. The intestinal microbiome is a collection of countless microorganisms such as bacteria, archaea, and viruses found in the gastrointestinal tract (Gupta et al., 2016). These microorganisms support various bodily processes, but they can be impaired by environmental factors and infectious diseases. FMT is highly effective in treating some of these infectious diseases. For example, it is up to 90% effective in curing recurrent infections of Clostridium difficile bacteria (Wang et al., 2019).
Recent research has extended the potential applications of FMT to address the symptoms of Autism Spectrum Disorders (ASDs). This diverse group of neurodevelopmental disorders typically leads to distinct patterns of behavior (difficulty in deviating from routines, repetitive movements, and fixations on specific objects or activities) and other social communication issues that impair one’s ability to hold a conversation or detect various social cues (“Autism Spectrum Disorder,” 2018). ASDs affect approximately one in fifty-nine individuals in the United States (Sharon et al., 2019). Many studies indicate a link between abnormal gut microbiota and ASD (Kang et al., 2019). Children with ASD who experience food sensory issues are more likely to face gastrointestinal problems due to deficits in calcium and protein intake. There are not many medical treatments available for these symptoms of ASD (Kang et al., 2019). Behavioral therapy can help improve social skills and issues with communication, but it does not address physical problems in the body. This is where FMT comes into play.
A study conducted by researchers at Arizona State University found promising results when combining FMT with bowel cleanses and antibiotics to treat children with ASD. After an eighteen-week trial, they observed an 80% reduction in gastrointestinal symptoms of ASD. When they re-evaluated participants two years later they found significant improvements in gastrointestinal and behavioral symptoms (Kang et al., 2019). These findings found support in subsequent studies that investigated the impacts of FMT on gastrointestinal symptoms and metabolic profiles of people with ASD (Martínez-González & Andreo-Martínez, 2020). However, further research is needed to validate this link between FMT and the improved health of patients with ASD. These additional studies should consider the diverse spectrum of ASD severity and the differences in methodologies used to measure ASD behaviors (Martínez-González & Andreo-Martínez, 2020).
These results are not only exciting because they can help such a large number of people, but also because they highlight the potential of treatments derived from readily available materials. The world is in an exciting era of medical innovation and amazingly complex medical technology, but FMT serves as a reminder that we don't always need highly specialized tools to start helping patients in need. Sometimes, using what we already have – in this case, an abundance of human fecal matter – can lead to significant medical breakthroughs.
References
Gupta, S., Allen-Vercoe, E., & Petrof, E. O. (2016). Fecal microbiota transplantation: in perspective. Therapeutic Advances in Gastroenterology, 9(2), 229–239. https://doi.org/10.1177/1756283X15607414
Kang, D. W., Adams, J. B., Coleman, D. M., Pollard, E. L., Maldonado, J., McDonough-Means, S., Caporaso, J. G., & Krajmalnik-Brown, R. (2019). Long-term benefit of Microbiota Transfer Therapy on autism symptoms and gut microbiota. Scientific Reports, 9(1), 5821. https://doi.org/10.1038/s41598-019-42183-0
Martínez-González, A. E., & Andreo-Martínez, P. (2020). Prebiotics, probiotics and fecal microbiota transplantation in autism: A systematic review. Revista de psiquiatria y salud mental, 13(3), 150–164. https://doi.org/10.1016/j.rpsm.2020.06.002
Autism Spectrum Disorder. (2018, January 6). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/autism-spectrum-disorder/symptoms-causes/syc-20352928
Sharon, G., Cruz, N. J., Kang, D. W., Gandal, M. J., Wang, B., Kim, Y. M., Zink, E. M., Casey, C. P., Taylor, B. C., Lane, C. J., Bramer, L. M., Isern, N. G., Hoyt, D. W., Noecker, C., Sweredoski, M. J., Moradian, A., Borenstein, E., Jansson, J. K., Knight, R., Metz, T. O., … Mazmanian, S. K. (2019). Human Gut Microbiota from Autism Spectrum Disorder Promote Behavioral Symptoms in Mice. Cell, 177(6), 1600–1618.e17. https://doi.org/10.1016/j.cell.2019.05.004
Wang, J. W., Kuo, C. H., Kuo, F. C., Wang, Y. K., Hsu, W. H., Yu, F. J., Hu, H. M., Hsu, P. I., Wang, J. Y., & Wu, D. C. (2019). Fecal microbiota transplantation: Review and update. Journal of the Formosan Medical Association, 118 Suppl 1, S23–S31. https://doi.org/10.1016/j.jfma.2018.08.011