Abstract:
Photoacoustic imaging is a technique in which contrast agents absorb photon energy and emit signals that can be analyzed by ultrasound transducers. This method allows for unprecedented depth imaging that can provide a non-invasive alternative to current diagnostic tools used to detect internal tissue inflammation.1 The Rice iGEM team strove to use photoacoustic technology and biomarkers to develop a noninvasive method of locally detecting gut inflammation and colon cancer. As a first step, we genetically engineered Escherichia coli to express near-infrared fluorescent proteins iRFP670 and iRFP713 and conducted tests using biomarkers to determine whether expression was confined to a singular local area.
Introduction:
In photoacoustic imaging, laser pulses of a specific, predetermined wavelength (the excitation wavelength) activate and thermally excite a contrast agent such as a pigment or protein. The heat makes the contrast agent contract and expand producing an ultrasonic emission wavelength longer than the excitation wavelength used. The emission wavelength data are used to produce 2D or 3D images of tissues that have high resolution and contrast.2
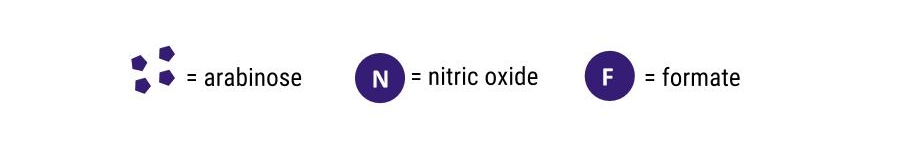
The objective of this photoacoustic imaging project is to engineer bacteria to produce contrast agents in the presence of biomarkers specific to gut inflammation and colon cancer and ultimately to deliver the bacteria into the intestines. The bacteria will produce the contrast agents in response to certain biomarkers and lasers will excite the contrast agents, which will emit signals in local, targeted areas, allowing for a non-invasive imaging method. Our goal is to develop a non-invasive photoacoustic imaging delivery method that uses engineered bacteria to report gut inflammation and identify colon cancer. To achieve this, we constructed plasmids that have a nitric-oxide-sensing promoter (soxR/S) or a hypoxia-sensing promoter (narK or fdhf) fused to genes encoding near-infrared fluorescent proteins or violacein with emission wavelengths of 670 nm (iRFP670) and 713 nm (iRFP713). Nitric oxide and hypoxia, biological markers of gut inflammation in both mice and humans, would therefore promote expression of the desired iRFPs or violacein.3,4
Results and Discussion
Arabinose
To test the inducibility and detectability of our iRFPs, we used pBAD, a promoter that is part of the arabinose operon located in E. coli.5 We formed genetic circuits consisting of the pBAD expression system and iRFP670 and iRFP713 (Fig. 1a). AraC, a constitutively produced transcription regulator, changes form in the presence of arabinose sugar, allowing for the activation of the pBAD promoter.
Fluorescence levels emitted by the iRFPs increased significantly when placed in wells containing increasing concentrations of arabinose (Figure 2). This correlation suggests that our selected iRFPs fluoresce sufficiently when promoters are induced by environmental signals. The results of the arabinose assays showed that we successfully produced iRFPs; the next steps were to engineer bacteria to produce the same iRFPs under nitric oxide and hypoxia.
Nitric Oxide
The next step was to test the nitric oxide induction of iRFP fluorescence. We used a genetic circuit consisting of a constitutive promoter and the soxR gene, which in turn expresses the SoxR protein (Figure 1b). In the presence of nitric oxide, SoxR changes form to activate the promoter soxS, which activates the expression of the desired gene. The source of nitric oxide added to our engineered bacteria samples was diethylenetriamine/nitric oxide adduct (DETA/NO).
Figure 3 shows no significant difference of fluorescence/OD600 between DETA/NO concentrations. This finding implies that our engineered bacteria were unable to detect the nitric oxide biomarker and produce iRFP; future troubleshooting includes verifying promoter strength and correct sample conditions. Furthermore, nitric oxide has an extremely short half-life of a few seconds, which may not be enough time for most of the engineered bacteria to sense the nitric oxide, limiting iRFP production and fluorescence.
Hypoxia
We also tested the induction of iRFP fluorescence with the hypoxia-inducible promoters narK and fdhf. We expected iRFP production and fluorescence to increase when using the narK and fdhf promoters in anaerobic conditions (Figure 1c and d).
However, we observed the opposite result. A decreased fluorescence for both iRFP constructs in both promoters was measured when exposed to hypoxia (Figure 4). This finding suggests that our engineered bacteria were unable to detect the hypoxia biomarker and produce iRFP; future troubleshooting includes verifying promoter strength and correct sample conditions.
Future Directions
Further studies include testing the engineered bacteria co-cultured with colon cancer cells and developing other constructs that will enable bacteria to sense carcinogenic tumors and make them fluoresce for imaging and treatment purposes.
Violacein has anti-cancer therapy potential
Violacein is a fluorescent pigment for in vivo photoacoustic imaging in the near-infrared range and shows anti-tumoral activity6. It has high potential for future work in bacterial tumor targeting. We have succeeded in constructing violacein using Golden Gate shuffling7 and intend to use it in experiments such as the nitric oxide and hypoxia assays we used for iRFP670 and 713.
Invasin can allow for targeted cell therapy
Using a beta integrin called invasin, certain bacteria are able to invade mammalian cells.8-9 If we engineer E. coli that have the beta integrin invasion as well as the genetic circuits capable of sensing nitric oxide and/or hypoxia, we can potentially allow the E. coli to invade colon cells and release contrast agents for photoacoustic imaging or therapeutic agents such as violacein only in the presence of specific biomarkers.10 Additionally, if we engineer the bacteria that exhibit invasin to invade colon cancer cells only and not normal cells, then this approach would potentially allow for a localized targeting and treatment of cancerous tumors. This design allows us to create scenarios with parameters more similar to the conditions observed in the human gut as we will be unable to test our engineered bacteria in an actual human gut.
Acknowledgements:
The International Genetically Engineered Machine (iGEM) Foundation (igem.org) is an independent, non-profit organization dedicated to education and competition, the advancement of synthetic biology, and the development of an open community and collaboration.
This project would not have been possible without the patient instruction and generous encouragement of our Principal Investigators (Dr. Beth Beason-Abmayr and Dr. Jonathan Silberg, BioSciences at Rice), our graduate student advisors and our undergraduate team. I would also like to thank our iGEM collaborators.
This work was supported by the Wiess School of Natural Sciences and the George R. Brown School of Engineering and the Departments of BioSciences, Bioengineering, and Chemical and Biomolecular Engineering at Rice University; Dr. Rebecca Richards-Kortum, HHMI Pre-College and Undergraduate Science Education Program Grant #52008107; and Dr. George N. Phillips, Jr., Looney Endowment Fund.
If you would like to know more information about our project and our team, please visit our iGEM wiki at 2016.igem.org/Team:Rice.
References
- Ntziachristos, V. Nat Methods. 2010, 7, 603-614.
- Weber, J. et al. Nat Methods. 2016, 13, 639-650.
- Archer, E. J. et al. ACS Synth. Biol. 2012, 1, 451–457.
- Hӧckel, M.; Vaupel, P. JNCI J Natl Cancer Inst. 2001, 93, 266−276.
- Guzman, L. M. et al. J of Bacteriology. 1995, 177, 4121-4130.
- Shcherbakova, D. M.; Verkhusha, V. V. Nat Methods. 2013, 10, 751-754.
- Engler, C. et al. PLOS One. 2009, 4, 1-9.
- Anderson, J. et al. Sci Direct. 2006, 355, 619–627
- Arao, S. et al. Pancreas. 2000, 20, 619-627.
- Jiang, Y. et al. Sci Rep. 2015, 19, 1-9.